Project Description
Our group began research in 2008 in the area of traumatic brain injury (TBI) when we began our collaboration with Dr. Ross Zafonte, Director of the Spaulding Rehabilitation Center. Dr. Zafonte is also principal investigator of the Harvard Clinical Defense Consortium Site on post-traumatic stress disorder (PTSD) and TBI, along with Drs. Roger Pitman and Martha Shenton who are co-principal investigators. These investigators are part of a large 10 site PTSD/TBI Clinical Consortium funded by the Department of Defense Psychological Health/Traumatic Brain Injury Research Program, and headed by Dr. Murray Stein at the University of San Diego. Members of the 10 site Clinical Consortium are conducting research studies with the aim of preventing and treating PTSD and TBI, two common but poorly understood disorders that affect millions of individuals, both military and civilian.
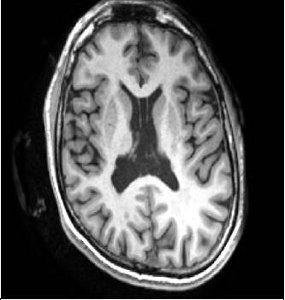
A 1.5mm coronal slice showing large cavum septum pellucidum visible within the lateral ventricles of the brain in a TBI patient.
Of particular note here, TBI is the signature injury of soldiers returning from Iraq and Afghanistan, with 59% of the soldiers treated at Walter Reed Hospital being diagnosed with TBI (80% of the cases are “mild”). The most common brain injury is “diffuse axonal injury”, which involves injury to white matter in the brain, or to the cables that connect neurons in the brain, with neurons being gray matter in the brain, and thought to be the processing centers of the brain. There are difficulties, however, in diagnosing mild cases of TBI because computerized tomography (CT), and conventional magnetic resonance imaging (MRI) are not able to detect diffuse axonal injury and these measures thus end up underestimating injuries and are poorly correlated with outcome. Additionally TBI and PTSD share similar symptoms and both can be present in the same individual. One study, in fact, shows a 43.9% overlap between the two disorders.
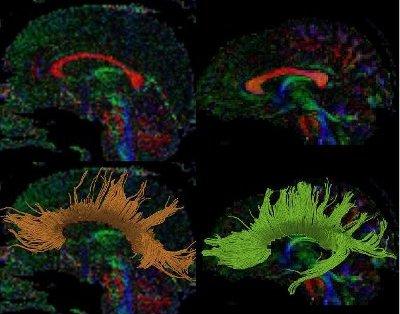
Note the thinning of the corpus callosum (top left in red) in the Traumatic Brain Injury patients compared with the Healthy Control on the right. Note also the 3D reconstruction of the fiber bundles of the corpus callosum on the bottom panel which shows fewer fiber bundles in the TBI patient (bottom left) compared with the Healthy Control (bottom right).
Our group has worked over the past decade to develop and to apply sensitive measures of white matter pathology in the living brain using relatively new techniques known as diffusion tensor and diffusion weighted imaging. This work is being conducted in conjunction with Dr. Carl-Fredrik Westin, Director of the Laboratory of Mathematical Imaging. Our group is also working with members of the Martinos Center at Massachusetts General Hospital, including Drs. Bruce Rosen, Karl Helmer, and Andre Van der Kouwe, to extract information from susceptibility weighted images to measure micro-hemorrhages in the brain, which may be important in understanding TBI. This latter work is also supported by the Clinical Consortium as part of the Neuroimaging Leadership Core, headed by Drs. Shenton, Kikinis and Rosen. A large database for all of the images is available at Washington University, and headed by Dr. Daniel Marcus who is also a member of the Neuroimaging Leadership Core for the Clinical Consortium sites.
Our goal is to develop biomarkers of white matter pathology that can be used for the diagnosis, prognosis, and monitoring of therapeutic efficacy in clinical trials of TBI. To this end, and as part of the Clinical Consortium, images from subject participants from all 10 sites will be acquired from both military and civilian populations to characterize better diffusion axonal injury in mild cases as well as in more moderate and severe cases of TBI. Our group is also working with Dr. Connie Duncan to evaluate both PTSD and TBI by investigating brain indices that include electroencephalography, and MRI and diffusion images of the brains of soldiers returning from Iraq and Afghanistan and being treated at Walter Reed Hospital. In addition, our group is leading a pilot project with collaborators at Brigham and Women’s Hospital, including Dr. Emily Stern, and Dr. Ross Zafonte at Spaulding Rehabilitation Center, to combine a PET ligand associated with detecting neuroinflammation in the brain with diffusion imaging in order to understand better the role of neuroinflammation in the early phases of TBI. In this sample the focus is on mild-complicated TBI, i.e., cases where there is an observed abnormality on CT or conventional MRI.
Other work by our group includes research supported by a Soldier’s Award grant from the Center for Integration of Medicine and Innovative Technology (CIMIT) to Dr. Sylvain Bouix to develop a white matter atlas of TBI to characterize better diffuse axonal injury in the brain. The hope is that we will be able to create a brain atlas where new cases can be compared to highlight regions of impairment, such as, for example, thinning of the corpus callosum that may indicate shearing of axons in this region. Impairments such as these could then be followed up to determine which cases recover, which evince more prolonged recovery, and which are more amenable to new treatments such as neuroprotective agents.
Additionally, members of our group are working with Dr. Robert Stern and his colleagues, including Drs. Ann McKee and Robert Cantu and Mr. Chris Nowinski at the Center for the Study of Traumatic Encephalopathy at Boston University School of Medicine to investigate the chronic effects of mild concussive injuries in sports related TBI. This work is particularly important as it focuses on mild cases of TBI that involve repetitive injury to the brain in order to determine the long term consequences. Currently these collaborators, along with Dr. Alex Lin who is focusing on magnetic resonance spectroscopy, are funded by the first R01 grant from the National Institute of Neurological Diseases and Stroke (NINDS) to investigate chronic traumatic encephalopathy in retired National Football Players. Work is also being conducted with Drs. Inga Koerte, Ertl-Wagner, Maximilian Reiser, Ross Zafonte, Marc Muehlmann, David Kaufmann, and Elisabeth Hartl on soccer players and the effects of subconcussive blows to the head, and pre and post-hockey season and the effects of both subconcussive and concussive blows to the head. The latter work includes Drs. Paul Echlin, Inga Koerte and other members of the research team.






Comments are closed.